Psoriasis
- Non-communicable
- Autoimmune
- Skin
Psoriasis (also known as PsO) is a chronic, immune-mediated inflammatory disease which primarily affects the skin and joints and is characterized by scaly, erythematous plaques which are often pruritic. It is a common skin disorder with genetic underpinnings, affecting approximately 2% of the population and may also be influenced by environmental factors. In most cases, psoriasis also affects a patient’s quality of life, is often accompanied by depression and may also be associated with other inflammatory disorders such as inflammatory bowel disease, and coronary artery disease and a seronegative form of arthritis known as psoriatic arthritis. There are various treatment options available to psoriasis patients, ranging from topical steroidal based therapies, phototherapy and biological therapies which target specific immune components.
Clinical Features
There are several clinical manifestations of psoriasis, the most common being plaque psoriasis, also known as psoriasis vulgaris. Most patients experience moderate to severe psoriasis, affecting more than 5% of the body surface area (BSA) or specific areas of the body such as the hands, feet, face, or genitals.
There are multiple phenotypically distinct types of psoriasis which have been identified, primarily based on morphologic features:
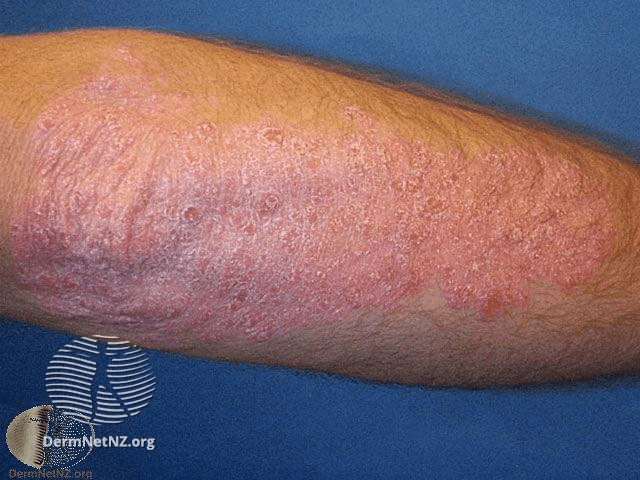
Plaque psoriasis
The most common form of the disease, affecting up to 90% of all patients. Plaque psoriasis, or psoriasis vulgaris, is characterized by well defined, round, erythematous plaques on the surface of the skin and located on the limbs, scalp and buttocks. It is likely that psoriasis vulgaris will eventually be classed as several phenotypic and genetically distinct conditions, given the variability observed with response to therapy, particularly with targeted biological agents.
Guttate psoriasis
This acute form of psoriasis predominantly occurs in individuals under the age of 30 and accounts for 2% of total cases. This variant manifests as many small (1-10mm) lesions and often follows a group A beta-hemolytic streptococci infection upper respiratory tract infection. Guttate psoriasis typically resolves within 3-4 months of onset, however, a significant proportion of patients also go on to develop chronic plaque psoriasis.
Pustular psoriasis
Also known as von Zumbusch psoriasis, this generalized acute form of the disease is uncommon and severe. It is characterized by small, painful, widespread pustules and typically accompanied by fever.
Flexural
Flexural, or inverse psoriasis, is characterised by lesions in the skinfolds and primarily affects the flexures. They are distinct from classical psoriasis plaques and are red, shiny and devoid of scaling.
Erythroderma
This form can develop acutely or gradually from chronic plaque psoriasis. Erythrodermic psoriasis typically covers the whole body surface while fever and
malaise
Malaise
General feeling of discomfort or unease, usually an early indicator for other symptoms to follow.
are also common. There is generalized erythema and can be life threatening in severe cases. It can also result from other diseases including atopic dermatitis and cutaneous T-cell lymphoma.
Nail Psoriasis
Nail involvement may be present across all types of psoriasis, with around 50% of psoriasis patients experiencing distinctive nail changes related to the disease. This includes pitting, oil spot formation and onycholysis (nail plate separation). This manifestation is also known as psoriatic onychodystrophy and occurs most commonly in patients with psoriatic arthritis.
Palmoplantar pustulosis
This form presents as yellow-brown, sterile pustules on the palms and soles and is associated with approximately 25% of all cases of psoriasis vulgaris. It is predominantly present in the female population (9:1 ratio of women to men) who are current or have a history of smoking. Following genetic studies which have demonstrated a lack of association with markers of psoriasis, it is now widely believed that this form may in fact be a comorbidity rather than a distinctive subtype of psoriasis.
Pathogenesis
To understand the pathogenesis of psoriasis, we must first outline the three main layers of the skin. The first is the epidermis, which consists primarily of epithelial cells known as keratinocytes. Second is the dermis, made up of collagens, fibroblasts, hair follicles, sebaceous glands and sweat glands which form the extracellular matrix. The third layer is known as the hypodermis, which contains subcutaneous adipose tissue and stromal cells. Psoriasis is characterised by dysfunctional differentiation and growth of keratinocytes, with cutaneous inflammation a result of infiltration of CD4+ T cells, CD8+ T-cells, Natural Killer cells and Natural Killer T cells. Occasionally neutrophils form a large proportion of the leucocytic infiltrate from the innate immune response, particularly in generalized pustular disease. There are two different cell types which interact in the formation of a psoriatic lesion; the keratinocytes in the epidermis and mononuclear
leukocytes.
Leukocytes
The white blood cells of the immune system, that defend the body against infectious diseases and foreign materials are known as leukocytes.
It is likely that keratinocytes are active participants in the recruitment and activation of
leukocytes
Leukocytes
The white blood cells of the immune system, that defend the body against infectious diseases and foreign materials are known as leukocytes.
in psoriatic lesions, with two sets of interactive cellular responses in the formation of a psoriatic lesion and potentially form a balance between the activation of innate and acquired immune cell types, with the factors produced by epidermal keratinocytes directly affecting T cells and dendritic cells, and vice versa. There is also a migration of epidermal Langerhans cells mediated by
cytokine
Cytokine
A broad category of small proteins released by a range of cells (including immune cells like macrophages, B lymphocytes, T lymphocytes) that act through receptors and are important for a range of processes including cell signaling, inhibition, maturation and proliferation.
response signaling in patients with early-onset psoriasis, probably in an attempt to maintain cutaneous immune homoeostasis. Resolution of psoriasis is accompanied by an observable decrease in infiltrating T cells, dermal and dendritic cells, Langerhans cells, neutrophils, as well as downregulated expression of the pro-inflammatory cytokines TNF-α, IFN-γ and IL-12/23-dependent genes. TNF-α is a key pro-inflammatory
cytokine
Cytokine
A broad category of small proteins released by a range of cells (including immune cells like macrophages, B lymphocytes, T lymphocytes) that act through receptors and are important for a range of processes including cell signaling, inhibition, maturation and proliferation.
of the innate immune response and is substantially increased in psoriasis, highlighted through consistently observable efficacy of anti-TNF biological therapies used to treat psoriasis. IL-23 is also important for the production of Th17 cells, which secrete IL-17 and has a fundamental role in the pathogenesis of psoriasis, with both cytokines also being targeted in current biological therapies.
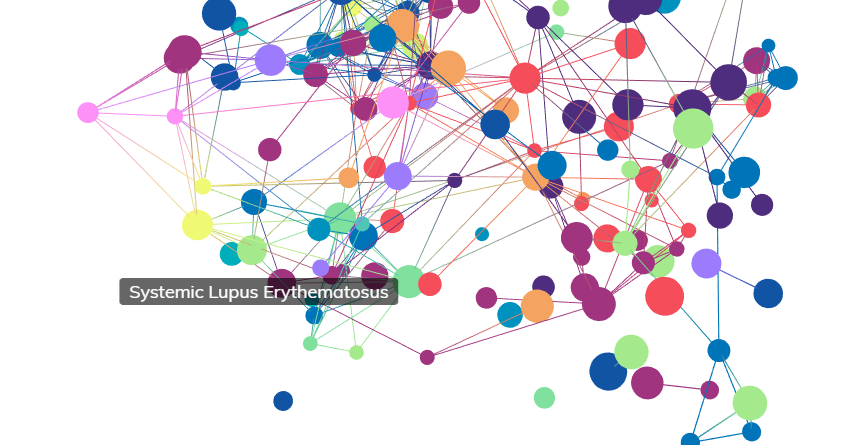
Comorbidities
There are a number of comorbidities associated with psoriasis not related to mortality and commonly resulting in severe impairment of quality of life. Notably, psoriasis is linked with lack of self-esteem and increased prevalence of mood disorders including depression. Many clinical studies investigating treatments for psoriasis use instruments generated to measure aspects of disease on quality of life such as Dermatology Life Quality Index (DLQI), Perceived Quality of Life Scale (PQOL) and Psoriasis Disability Index (PDI) scores. The prevalence of depression in patients with psoriasis may be as high as 60%. Comorbidities of psoriasis also include cardiovascular disease and a seronegative arthritis known as psoriatic arthritis. Even after correcting for a number of key risk factors for heart disease such as smoking, diabetes, obesity and hypertension, the probability of myocardial infarction is higher in individuals who suffer from moderate to severe psoriasis. Psoriasis has also been linked to a number of systemic disorders such as Crohn’s disease, multiple sclerosis, type 2 diabetes, metabolic syndrome and some types of cancer. It is unclear however whether cancers, particularly lymphoma and skin cancer, are directly attributed to psoriasis or to its treatment. For example, excessive treatment with photochemotherapy and the subsequent use of ciclosporin can result in non-melanoma skin cancer.
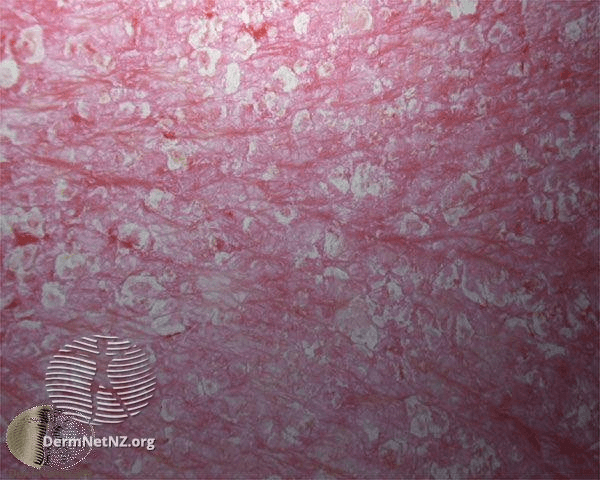
Cellular Characteristics
The primary histological features of psoriasis include the presence of neutrophils in the stratum corneum and substantial mononuclear infiltrates in the epidermis. There is also a clear infiltration of mononuclear
leukocytes
Leukocytes
The white blood cells of the immune system, that defend the body against infectious diseases and foreign materials are known as leukocytes.
into the dermis and elongated blood vessels in the papillary dermal region. This marked dilation of blood vessels manifests as the visible redness seen in psoriatic skin lesions. Endothelial cells are activated in psoriatic lesions, as is indicated by upregulation of adhesion molecule-1 (ICAM-1/CD54), vascular cell adhesion molecule-1 (VCAM-1/CD106) and E-selectin (CD62E). One of the hallmarks of psoriasis is the significantly raised level of Vascular Endothelial Growth Factor (VEGF) in plaques of psoriasis. Serum concentration of VEGF correlates with the clinical severity of the disease. The VEGF signaling pathway is modulated by TNF-α.
Genetics
There are at least 9 chromosomal loci identified to be associated with psoriasis (PSORS1-9). Of these 9 loci, PSOR1 (the human leucocyte
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
HLA-Cw6 allele) at 6p21, has been identified as the major susceptibility locus for psoriasis and accounts for 35% of the heritability of psoriasis. Association with PSOR1 has been replicated in effectively all genetic linkage studies of psoriasis. The phenotypic variants of psoriasis are genetically heterogeneous at least at the level of PSORS1. Guttate psoriasis is associated with PSORS1 whereas palmoplantar pustulosis and late onset psoriasis are not. There have been strong associations reported with HLA-Cw6 in patients with early onset psoriasis, compared with late onset disease. PSORS8 is also notable as psoriasis and Crohn’s disease are frequently observed together. Despite this, several studies have failed to find an association between psoriasis and the CARD15/NOD2 mutation which has been linked to Crohn’s disease. Missense mutations in the IL-23 receptor gene and single nucleotide polymorphisms in the untranslated IL-12B region identify psoriasis risk genes. There is certainly a genetic component to psoriasis, however the exact locations of susceptibility have not been fully established. The difficulty of confirming psoriasis susceptibility loci may be linked to the heterogeneity among different populations. Approximately 30% of individuals with psoriasis vulgaris have a first degree relative affected by the disease. If both of the parents and a sibling are affected, there is a further 50% chance the child will develop psoriasis vulgaris.
Treatment
There are a variety of treatment options which are indicated for the treatment of psoriasis. The administration of these treatment options depends on many factors such as severity of disease and effectiveness of early treatments:
Topical Treatments
Topically administered treatments such as salicylic acid and coal tar are used to treat the disease locally and are typically given as a first line of treatment in newly diagnosed patients. Many of these treatments can be purchased over the counter.
Phototherapy
There are two main types of phototherapy used to treat psoriasis - Ultraviolet B (UVB) and Psoralen Ultraviolet Long Wave Radiation (PUVA) therapy. Treatment involves exposing affected skin to an artificial light source for a set length of time on a regular schedule. UVB is safe and cost-effective, can be administered outside of the clinic and is usually given 2 to 3 times a week. PUVA therapy is effective in most patients, with a potential for long remissions. However, long-term PUVA treatment in Caucasians has been associated with an increased risk of squamous cell carcinoma and possibly malignant melanoma.
Systemic Therapies
There are a number of established systemic therapies used to treat psoriasis which cannot be managed by topical treatment including methotrexate, cyclosporin A (CyA) and acitretin. Methotrexate is an immunosuppressive agent and commonly used as an effective treatment for moderate to severe psoriasis. However, methotrexate also has the has a number of contraindications and the potential for hepatotoxicity. It is a class of drugs known as disease-modifying antirheumatic drugs (DMARDs), also indicated for psoriatic arthritis and rheumatoid arthritis. CyA is another immunosuppressive medication which can work rapidly and effectively in many patients. There are also concerns regarding long-term CyA treatment such as impaired renal function, hypertension and increased incidence of some malignancies. Acitretin is an effective systemic agent for the treatment of psoriasis and is not immunosuppressive. Acitretin is frequently used in combination therapy with UVB or PUVA. Because acitretin is teratogenic, it’s use is substantially limited in female patients of childbearing potential. Apremilast is an oral phosphodiesterase 4 (PDE4) inhibitor which works intracellularly to regulate inflammatory mediators, including pathways relevant to the pathogenesis of psoriasis. The ESTEEM-1 trial was a phase III, multicenter, double-blind, placebo-controlled study 844 adults were randomized (2:1) to apremilast or placebo. At week 16, the placebo group switched to apremilast through week 32, followed by a randomized treatment withdrawal phase to week 52. At week 16, significantly more patients taking apremilast achieved Psoriasis Area and Severity Index (PASI)-75, defined as <75% improvement in the PASI response relative to baseline, of 33.1% versus placebo (5.3%, P < 0.0001; primary end point). 61.0% of patients rerandomized to apremilast at week 32 achieved PASI-75 at week 52 versus 11.7% rerandomized to placebo. Most adverse events reported were mild/moderate in severity.
Biologic Agents
These therapies are proteins extracted from animal tissue or produced by recombinant
DNA
Deoxyribonucleic Acid (DNA)
The nucleic acid molecule that contains all the genetic information regarding the development and functioning of all living organisms is known as deoxyribonucleic acid.
technology. The latest biologic therapies for psoriasis target its immune components and may predict potential treatments for other inflammatory human diseases. After patients have been initiated on a biologic treatment, it is likely they will go on to further biologics or systemic therapies. Patients treated with biologic agents must be periodically re-evaluated for the development of new symptoms including infection and malignancy. The administration of live vaccines must be avoided in patients being treated with biologics.
Alefacept is a biologic therapy targeting CD2 on memory-effector T lymphocytes, thereby inhibiting the activation and proliferation of these cells. In an international multicenter, randomized, double-blind, parallel-group study comparing once-weekly alefacept 7.5 mg IV or placebo for two 12-week treatment courses, 28% of patients treated with alefacept achieved ≥75% reduction in PASI, compared with 8% of placebo-treated patients (P < 0.001). It was approved for the treatment of adult patients with moderate to severe chronic plaque psoriasis who are candidates for systemic agents or phototherapy but has since been discontinued due to an increased risk of systemic disease and malignancy associated with treatment.
Efalizumab is a monoclonal antibody targeting the CD11a subunit of LFA-1 and interferes with T cell activation. In a phase III, randomized, double-blind trial, 498 patients received subcutaneous 1 or 2 mg/kg/week efalizumab or placebo for 12 weeks. At week 12, 39% and 27% of efalizumab-treated patients (1 and 2 mg/kg, respectively) achieved PASI-75 (vs 2% placebo; P < 0.001, both dose groups). Efalizumab-treated patients who achieved <PASI-75 were re-randomized to a second 12-week course of treatment. At week 24, an additional 20% of efalizumab-treated patients achieved PASI-75 (vs placebo 7%, P = 0.018). Efalizumab was also discontinued due to an increased risk of progressive multifocal leukoencephalopathy (PML) linked to treatment.
There has been a lot of success using anti-TNF biological therapies to treat psoriasis, which is unsurprising given the elevated levels of TNF-α in both the affected skin and serum of patients with psoriasis. Adalimumab was the first fully human anti-TNF-α monoclonal antibody and is currently approved for psoriasis, juvenile rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis, adult rheumatoid arthritis, and Crohn's disease. In a multicenter randomized study of 1212 patients to receive adalimumab (40 mg) or placebo every other week for the first 15 weeks, 71% (578 of 814) of adalimumab- and 7% (26 of 398) of placebo-treated patients achieved PASI-75 at week 16.
Etanercept has demonstrated efficacy in the treatment of several inflammatory diseases and is currently approved for treatment of moderate to severe plaque psoriasis, psoriatic arthritis, rheumatoid arthritis, juvenile rheumatoid arthritis, and ankylosing spondylitis. A randomized, double-blind, placebo-controlled, 12-week study assessed the efficacy and safety of etanercept (25 mg twice-weekly subcutaneous injections) or placebo in 60 patients with psoriatic arthritis and psoriasis. The median PASI improvement was 46% in etanercept-treated patients versus 9% in placebo-treated patients.
Infliximab binds to both the soluble and the transmembrane TNF-α molecules, thereby neutralizing the effects of TNF-α. In a phase III, multicenter, double-blind trial, 378 patients with moderate-to-severe plaque psoriasis were allocated in a 4:1 ratio to receive infusions of either infliximab 5 mg/kg or placebo at weeks 0, 2, and 6, then every 8 weeks to week 46. At week 24, placebo-treated patients crossed over to infliximab treatment. At week 10, 80% of patients treated with infliximab achieved PASI-75 and 57% achieved at least a PASI 90, compared with 3% and 1% in the placebo group, respectively (p<0.0001). At week 24, PASI 75 (82% for infliximab vs 4% for placebo) and PASI 90 (58% vs 1%) were maintained (p<0.0001). At week 50, 61% achieved PASI 75 and 45% achieved PASI 90 in the infliximab group. Infliximab was generally well tolerated in most patients.
An important issue to consider with TNF inhibitors is the potential loss of efficacy over time. All of the TNF inhibitors carry the potential for an increased risk of infection with upper respiratory tract infections being the most common, however serious infections are uncommon. Treatment with TNF inhibitors should be avoided if possible in patients with chronic, serious, or recurring infections. The potential risk of melanoma, cutaneous T-cell lymphoma, and nonmelanoma skin cancer in patients treated with the TNF inhibitors has been raised by several case reports.
Epidemiology
Psoriasis is among the most prevalent immune-mediated skin disease in adults and affects about 25 million people in North America and Europe. The prevalence of psoriasis varies widely between different populations globally, with men and women affected equally. The prevalence in the UK is around 1.6%, 1.4% in Norway and 1.55% in Croatia, while in the USA estimates are closer to 4.6% and 4.7% in Canada. It generally affects Caucasians more commonly, with only 0.7% of American Blacks affected by psoriasis. In East Africa, the figure was 0.7% and in China only 0.3-0.4% were seen to be affected. High rates of psoriasis have been reported in people of the Faroe Islands, where one study found 2.8% of the population to be affected, whereas the prevalence of psoriasis is low in certain ethnic groups such as the Japanese, and may be absent altogether in aboriginal Australians and Indians from South America. It is estimated that there are 5.1 million people affected in Europe, 4.9 million in the USA and 2.5 million in Japan. Psoriasis can manifest at any stage in life, however, the mean age of onset for psoriasis vulgaris was recently estimated at 33 years, with 75% of cases occurring before the age of 463. There has been a bimodal age of onset observed in multiple studies, with peaks between 15 - 20 years and 55 - 60 years. The age of onset seems to be slightly earlier in women than in men. There is also a strong genetic component though environmental factors such as infections can play an important role in the onset of disease. Early onset disease accounts for more than 75% of cases. It is surprising to note that no significant changes in annual incidence rates were reported in these epidemiological studies given that psoriasis is a multifactorial disease with a suspected role of environmental factors contributing to disease onset. One of the common features of autoimmune conditions is a higher prevalence of females affected compared to males. However, there are no significant differences between male and female patients observed, only in the age of onset.
Additional Resources

The Psoriasis Association
The leading national charity and membership organisation for people affected by psoriasis in the UK. Through their work, they help people whose lives are affected by psoriasis and psoriatic arthritis. They do this through funding research, providing information and raising awareness.
What They Do:
• Offer good quality, reliable and independent information and advice.
Raise awareness of psoriasis and work with key health officials on strategic issues.
• Distribute copies of our members magazine 'Pso' to all Dermatology and Rheumatology departments in the UK.
• Represent the interests of members at a local and national level.
• Fund and promote research into the causes, nature and care of people with psoriasis.
https://www.psoriasis-association.org.uk/
The American Academy of Dermatology
The American Academy of Dermatology was founded in 1938. It is the largest, most influential and representative dermatology group in the United States. With a membership of more than 20,500, it represents virtually all practicing dermatologists in the United States, as well as a growing number of international dermatologists.
https://www.aad.org/public/diseases/scaly-skin/psoriasis/psoriasis
References
- "Lowes A & Michelle A - Pathogenesis and therapy of psoriasis. Nature. 2007; 22;445(7130):866-73."
- "Christophers E - Psoriasis - epidemiology and clinical spectrum. Clin Exp Dermatol. 2001; 26(4):314-20."
- "Griffiths CE & Barker JN - Pathogenesis and clinical features of psoriasis. Lancet. 2007; 370(9583):263-71."
- "Langley R, et al. - Psoriasis: epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005; 64(Suppl 2): ii18–ii23."
- "Menter A, et al. - Guidelines of care for the management of psoriasis and psoriatic arthritis. J Am Acad Dermat. 2008; 58(5):826-850"
- "Papp K, et al. - Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: Results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). Journal of the American Academy of Dermatology. 2015; 73(1): 37-49"
- "Krueger G - Clinical response to alefacept: results of a phase 3 study of intravenous administration of alefacept in patients with chronic plaque psoriasis. Journal of the European Academy of Dermatology and Venereology. 2003; 17: 17–24"
- "Leonardi C, et al. – Extended efalizumab therapy improves chronic plaque psoriasis: Results from a randomized phase III trial. Journal of the American Academy of Dermatology. 2005; 52 (3): 425-433"
- "Menter A, et al. - Adalimumab therapy for moderate to severe psoriasis: A randomized, controlled phase III trial. Journal of the American Academy of Dermatology. 2008; 58(1): 106-115"
- "Mease PJ, et al. - Etanercept in the treatment of psoriatic arthritis and psoriasis: a randomised trial. The Lancet. 2000; 253(9227): 385-390"
- "Reich K, et al. - Infliximab induction and maintenance therapy for moderate-to-severe psoriasis: a phase III, multicentre, double-blind trial. The Lancet. 2005; 366(9494): 1367-1374"