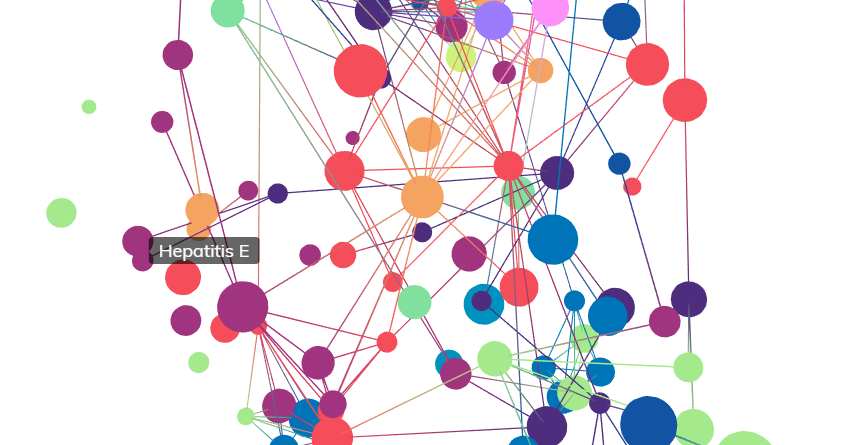
Hepatitis C
- Communicable
- Viral Infections (RNA)
- Flaviviridae
Hepatitis C virus (HCV) is a small single-stranded ribonucleic acid (RNA) virus of the Flaviviridae family of viruses and was first identified in 1989. Despite being a relatively simple virus, with a genome encoding only 11 proteins, HCV is a globally prevalent pathogen which affects over 185 million people worldwide. This represents approximately 2.8% of the population and infection may result in chronic liver disease. HCV can be transmitted in a number of ways including exposure to HCV-infected blood, vertical transmission (mother to child), infected needle stick exposure or unprotected sex. Most people infected with the virus initially present with no symptoms, though if left untreated, symptoms such as nausea, and can arise. As the disease progresses, individuals may ultimately develop liver damage, cirrhosis and end stage liver disease (ESLD). Among the various risk factors associated with chronic hepatitis C, an individual’s age, daily alcohol consumption, viral coinfection and gender all contribute to disease progression following infection. There has been significant progress made in the treatment options available for chronic HCV over the past decade, particularly with the development of direct acting antiviral agents, however these treatment options are expensive and efforts to develop an effective vaccine are still ongoing.
Clinical Features
Diagnosis of individuals infected with hepatitis C is particularly difficult due to the chronic nature of the disease and delayed onset of symptoms. This is further complicated by a variable rate of progression and a lack of reliable prognostic information available for patients. There are two main disease phases in the progression of HCV infection which determine the clinical features:
Acute Phase
The acute phase of disease in individuals recently exposed to HCV is often undiagnosed as symptoms rarely manifest or are mild in nature. Symptoms that are present in acute hepatitis may consist of
jaundice
Jaundice
Yellow discoloration of the skin, which also can result in exteme itchiness. Usually associated with liver diseases, such as viral hepatitis.
malaise
Malaise
General feeling of discomfort or unease, usually an early indicator for other symptoms to follow.
and nausea, with acute infection either being spontaneously cleared of
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
(the presence of HCV
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
genomes in the bloodstream) or, in most cases, developing into to chronic infection. There is a subset of patients with recently acquired HCV infection who present with clinically overt disease including
jaundice
Jaundice
Yellow discoloration of the skin, which also can result in exteme itchiness. Usually associated with liver diseases, such as viral hepatitis.
and these individuals are more likely to achieve viral clearance. Only 10-25% of infected patients in the adult population spontaneously resolve their infection, while the rest remain persistently viremic and asymptomatic. Liver cell injury develops in most infected patients within 15-50 days and is commonly associated with an increase in serum
alanine aminotransferase (ALT)
ALT
An enzyme which is dispursed through the bloodstream when liver or heart damage occurs.
levels. Elevated serum ALT levels indicate active liver disease, but these levels can fluctuate widely and it is not a reliable indicator of the presence or severity of the disease. Following 3 months of viral exposure, most infected subjects will begin to produce anti-HCV antibodies.
Chronic Phase
Hepatitis C is typically characterised by this extended chronic phase of disease, with the outcome of infection determined within six months of exposure. Spontaneous clearance of
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
once chronic disease develops is rare, and liver related symptoms such as
malaise
Malaise
General feeling of discomfort or unease, usually an early indicator for other symptoms to follow.
, fatigue, drowsiness, and muscle aches will likely begin to develop. Most chronic infections will result in
hepatitis and a degree of liver
fibrosis
Fibrosis
Excessive tissue forming to compansate during organ repair. This overcompansation can often serve to obstruct the organ from functioning properly.
which can be accompanied by symptoms such as fatigue. More severe complications and death occur in patients with
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
, which develops in approximately 15-20% of individuals with chronic
hepatitis C infection.
Given that the acute and early phase of chronic infection is often asymptomatic, the natural history of HCV infection can be difficult to assess. Less than 20% of patients with chronic infection develop symptoms initially, and these are usually nonspecific in nature such as
malaise
Malaise
General feeling of discomfort or unease, usually an early indicator for other symptoms to follow.
, muscle aches, mild fatigue and drowsiness. It is estimated that 74-86% of patients will have persistent
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
and a subset of these individuals are asymptomatic, and these individuals potentially represent a growing segment of candidates for anti-viral treatment. Patients may ultimately go on to develop advanced liver disease, though the duration of disease progression is typically long. Moreover, the time frame for this progression is highly variable. One third of individuals go on to develop serious liver disease less than 20 years after infection while on the other hand no progression is observed in another third of those infected beyond 30 years. While HCV infection may be associated with ESLD, a majority of adult patients will have persistent
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
without clinical manifestations related to liver disease. There are also four key factors which contribute to accelerated clinical progression including alcohol intake, human immunodeficiency virus (HIV) or hepatitis B virus (HBV) infection, age and gender.
Pathogenesis
The chronic viral persistence of HCV infection results from an inadequate immune response and an inability to eradicate infected cells. During the acute phase, viral clearance and control of replication is associated with a strong CD4+ helper and CD8+ cytotoxic T cell response. The natural target for HCV are
hepatocytes
Hepatocyte
A type of cell located in the liver which facilitates many liver functions, including protein storage and detoxification.
in the liver, however HCV is not
cytopathic
Cytopathic
An effect in which cells are changed structurally as a result of viral infection. This results in lysis of the host cell or cell death without lysis due to an inability to reproduce.
for the infected cell. HCV invades
hepatocytes
Hepatocyte
A type of cell located in the liver which facilitates many liver functions, including protein storage and detoxification.
and replicates within the
cytoplasm
Cytoplasm
Refers to all of the material within a cell which is enclosed by the cell membrane, except for the cell nucleus. The main components of the cytoplasm are cytosol and organelles (substructures within the cell).
after entering the host cell.
Replication of the virus in the infected
hepatocyte
Hepatocyte
A type of cell located in the liver which facilitates many liver functions, including protein storage and detoxification.
is extremely robust, and it is estimated that more than 10 trillion virion particles are produced per day, including during the chronic phase of infection. It was previously thought that only a small number of
hepatocytes
Hepatocyte
A type of cell located in the liver which facilitates many liver functions, including protein storage and detoxification.
become infected in the chronic phase but more recent studies suggest that more than 50% of these cells in infected individuals may harbour the virus. HCV
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
genomes appear in the host
plasma
Plasma
Blood plasma is the yellow-colored portion of the blood carrying cells and proteins throughout the body.
within a few days of infection and these levels typically peak at around the 6–10 week mark. An individual with poorly controlled
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
is a predictor for persistence of infection and this may result from a failure to generate detectable CD4+ and CD8+ T cell responses.
Control of
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
is associated with reduced levels of virus-specific CD4+ and CD8+ T cell responses and a marked increase in HCV replication, demonstrating the balance between viral genome clearance and programmed cell death to regulate the immune response. This rise in
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
likely represents the viral persistence associated with the late stages of acute phase
hepatitis C. Conversely, successfully controlled HCV infections result in durable T cell memory populations and could explain the lower rate of HCV persistence seen in previously exposed patients who have a history of resolving acute phase
hepatitis C.
This early T cell response plays a critical role in the control of HCV and the
pathogenesis
Pathogenesis
The biological mechanism that leads to a state of disease. It can refer to the origin and development of a disease, as well as whether it is recurrent, chronic and acute.
of liver disease. The ability of the virus to outpace the host T cell response likely contributes to the persistence of HCV infection and the quality of this early immune response to HCV likely play’s a key role in the overall outcome of the infection. A high viral load may contribute to a patient’s immune response becoming suppressed, however chronic infection may also be characterised by persistent
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
. Thus, levels of
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
do not necessarily correlate with either acute or chronic infection and although relevant to the outcome of anti-HCV therapy, it is not an ideal marker for measuring disease progression. The relatively weak CD8+ T cell response in the chronic phase appears to be insufficient to contain
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
and the genetic evolution of the virus, but sufficient to cause collateral damage through the release of inflammatory cytokines in the liver.
It is difficult to predict the disease course following HCV infection and the rate of progression varies considerably. A multispecific immune response to HCV epitopes (the targets recognised by the immune system) or those which are predominated by a CD4+ helper type 1 (Th1) response (rather than Th2 response), as well as a strong CD8+ cytotoxic T cell response, have resulted in improved viral clearance. As highlighted above in the Clinical Features section, the rate of fibrosis progression is also associated with the following factors: gender (higher in males), the age at infection (progression is more rapid in older patients aged > 40 years), coinfection with another virus such as HBV or HIV, and daily alcohol consumption (more rapid progression in those who consume > 50g/day).
Comorbidities
There are a number of disorders associated with HCV infection as well as factors which influence the manifestation of comorbidities. As outlined above in the Clinical Features section, HCV infection may lead to liver
fibrosis
Fibrosis
Excessive tissue forming to compansate during organ repair. This overcompansation can often serve to obstruct the organ from functioning properly.
,
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
and ESLD. The probability of HCV infected patients developing
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
over a 30-year period ranges from 13% to 46% for men and from 1% to 29% for women, approximately 20% overall. Alcohol consumption is a key factor in disease progression and liver fibrosis. Moreover, the incidence of ESLD is significantly higher in patients consuming 3 or more alcoholic drinks daily.
Another important factor is co-infection with other viruses, particularly HIV and HBV. HIV coinfection has been associated with accelerated progression of liver disease and decreased survival prior to highly active antiretroviral therapy (HAART) in the developed world. Patients co-infected with HBV have also been demonstrated more severe and accelerated liver disease than in those infected with HCV alone.
HCV infection can adversely affect a patient’s quality of life even in the absence of severe disease. Cryoglobulins (a type of immunoglobulin or antibody) can be found in up to half of hepatitis C patients, though only 10-15% experience symptomatic disease. HCV is a leading cause of type II cryoglobulinemia, with up to 90% of these patients presenting with HCV
viremia
Viremia
The presence of virus in the bloodstream leaving the rest of the body vulnerable to infection.
.
A higher incidence of non-Hodgkin's lymphoma has also been associated with HCV infection while Hepatocellular carcinoma (HCC), a form of liver cancer, affects up to 2.5% of patients with hepatitis C. This demonstrates yet another serious health burden attributable to HCV infection and the subsequent chronic liver damage associated with disease progression.
Cellular Characteristics
HCV is surrounded by a distinct icosahedral protective
protein
Protein
Large biomolecules, which consist of one or more long chains of amino acid residues. They perform a vast array of functions within organisms including transporting molecules, providing cellular structure and catalysising processes such as DNA replication.
shell encased in a
lipid envelope
Lipid Envelope
A protective layer that that contains viral proteins, usually including components which enable the virus to bind to the host cells.
approximately 60nm in size. It encodes key envelope glycoproteins, E1 and E2, as well as non-structural proteins NS2, NS3, NS4A, NS4B, NS5A, NS5B. The surface
protein
Protein
Large biomolecules, which consist of one or more long chains of amino acid residues. They perform a vast array of functions within organisms including transporting molecules, providing cellular structure and catalysising processes such as DNA replication.
CD81, expressed on cells such as B lymphocytes and
hepatocytes
Hepatocyte
A type of cell located in the liver which facilitates many liver functions, including protein storage and detoxification.
, has been shown to bind to E2.
A key function of CD4+ T cells is to secrete cytokines that modulate the activity
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
specific B cells and CD8+ cytotoxic T cells. CD4+ and CD8+ T cells recognise short
peptide
Peptide
A chemical compound consisting of at least two amino acids.
epitopes complexed with major histocompatibility complex (MHC) class II or class I molecules, respectively, on the cell surface of
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
-presenting cells such as B cells, dendritic cells and macrophages. Reduced
epitope
Epitope
A part of an antigen that is recognised by the immune system, specifically by antibodies, B cells, or T cells.
binding by MHC class I molecules caused by amino acid substitution has been described in some HCV specific CD8+ cytotoxic T cell epitopes. This effectively renders infected cells with this mutated
epitope
Epitope
A part of an antigen that is recognised by the immune system, specifically by antibodies, B cells, or T cells.
invisible to the relevant CD8+ T cells, as the MHC-
peptide
Peptide
A chemical compound consisting of at least two amino acids.
complex required for T cell receptor recognition is no longer expressed at the cell surface.
The CD4+ T cell response to HCV is typically detected by measuring the
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
-specific responses by proliferative mononuclear cells (MNCs) in the blood to recombinant HCV-encoded antigens in patients with
hepatitis C. Virally encoded peptides are usually synthesised by the infected host cell and normally follow the MHC class I
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
presentation pathway, which induces a CD8+ T cell response. The presence of lymphocytes within the functional cells of the liver, known as the hepatic
parenchyma
Parenchyma
The central tissue to bodily organs which are essential for their functioning.
, has been interpreted as evidence of immune-mediated damage in
hepatitis C patients.
It has been shown that viral clearance of acute
hepatitis C is more likely in cases displaying a CD4+ T helper type I (Th1) profile (characterised by production of cytokines IL-2 and IFN-γ) than in those producing a CD4+ T helper type 2 (Th2) profile (IL-4 and IL-10). Moreover, intrahepatic CD4+ T cells derived from patients with chronic
hepatitis C secrete predominantly Th1 cytokines, providing support for the recruitment and proliferation CD8+ T cells. A strong CD8+ T cell response in conjunction with sustained CD4+ T cell proliferation to multiple recombinant structural and non-structural viral proteins is seen in individuals resolving acute hepatitis C. Conversely, HCV
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
-driven proliferation in individuals who develop persistent infections is typically weak or absent compared with spontaneously resolving infections and permanent loss of this cellular proliferation during the acute phase predicts persistence.
Histological evaluation of a liver biopsy is the primary method for determining the extent of HCV related liver disease. Staging using histology remains the only reliable predictor of prognosis and the likelihood of disease progression. Though not considered mandatory to commence treatment, a biopsy may also help to rule out other causes of liver disease and is generally recommended for the assessment of newly diagnosed chronic HCV infection.
Genetics
The
hepatitis C virus is a member of the Hepacivirus genus of the Flaviviridae family and contains a positive-sense single-stranded
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
genome of about 10 kilobases, comprised of approximately 9600 base pairs. It encodes a single polypeptide precursor of 3011 amino acids which is cleaved to produce three structural and seven non-structural proteins. Viral replication occurs through an
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
polymerase encoded by the NS5B gene which lacks proofreading capacity and is error prone, resulting in the rapid evolution of diverse viral variants known as ‘quasispecies’.
The mutation rate within the HCV genome is approximately 1.5–2.0 x 10−3 base substitutions per genome site per year, and with a production of roughly 1010 to 1012 viral genomes per day in a chronically infected patient, leads to significant generation of these viral variants. The genomic diversity that results from these quasispecies presents a major challenge with respect to immune-mediated control of HCV. As described above in the Histology section, CD8+ T cells recognise short
peptide
Peptide
A chemical compound consisting of at least two amino acids.
epitopes complexed with MHC class I molecules on the cell surface of
antigen
Antigen
A structural molecule that is recognised by the adaptive immune system, binding to a T cell receptor (TCR) or B cell receptor (BCR) or antibody.
-presenting cells and these epitopes may be lost, resulting in impaired binding to MHC molecules. Consequently, the diversity of these viral variants can be exploited to evade recognition by CD8+ T cells, leading to the development of ‘escape mutations’.
There are seven major genotypes of HCV which are distinct but related (1 to 7) and 11 common subtypes (1a-c, 2a-c, 3a, 3b, 4a, 5a, and 6a), although the total number of subtypes could be as high as 100. Strains of the virus that belong to different genotypes differ at 30-35% of nucleotide sites while those that belong to the same subtype differ at < 15% of nucleotide sites.
Treatment
There has been significant progress made in the treatment options available for chronic hepatitis C over the past decade. Consensus guidelines for treatment however remain ambivalent, given the variability of symptomatic disease. As described above in the Clinical Features section, symptomatic patients who are seropositive but are otherwise healthy represent a growing segment of treatment candidates.
For chronic
hepatitis C patients, sustained virologic response (SVR) is the major surrogate for clinical outcomes such as improved survival, while patient reported outcomes (PROs) are also being increasingly used in clinical trials. The success of
hepatitis C therapies can also be measured in terms of a biochemical response (for example ALT levels), as well as the detection of viral
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
to assess virologic response.
Not long after the discovery of HCV in 1989, interferon (IFN) based monotherapy became the standard of care, followed by the introduction of ribavirin (RBV) combination therapy in the 1990s. More recently, the development of direct acting antivirals (DAAs) has not only significantly improved response rates but also patient quality of life, as IFN and RBV therapy are associated with various symptoms including fatigue and depression.
Interferon Therapy
Interferon-based therapy was introduced even before the discovery of HCV and remains an important secondary prevention agent in HCV infected patients. There have been a number of interferons used since HCV was identified, each appearing to demonstrate similar efficacy. In 1989, the first cases of successful treatment of HCV with interferon alpha (IFN-α) were reported. IFN-α monotherapy was associated with initial response rates as high as 40%, however the sustained response rates were less than half this, especially in genotypes 1a or 1b which are the most prevalent genotypes in the United States and western Europe4. In the early 2000s, a pegylated (polyethylene glycol conjugated) form of interferon (PEG-IFN) alpha was developed, reducing the number of injections required.
Combination with Ribavirin
In the late 1990s, ribavirin (RBV), a nucleoside inhibitor which inhibits viral
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
synthesis, was approved in combination with interferon for the treatment of HCV. Recommendations from 1999 guidelines suggested that previously untreated persons should receive combination therapy. Two large, prospective clinical trials demonstrated that the combination of IFN-α and RBV significantly increases the percentage of previously untreated patients who have a sustained virologic response, from 16% to 40%. Treatment with IFN-α or a combination of IFN-α and RBV has been associated with a reduced risk of
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
, HCC and ESLD. Treatment for chronic
hepatitis C however has been shifting rapidly and moving to IFN-α and RBV-free oral regimens which are simpler and shorter to administer with very high efficacy rates and better tolerability.
Direct Acting Antivirals
The development of first generation DAAs marked a substantial improvement in SVR rates. In 2011, the first generation of protease inhibitors (boceprevir and telaprevir) were approved for use in a triple combination with IFN-α and RBV in patients with HCV genotype 1. Although gains in efficacy were observed with these regimens with increasingly better SVR rates, the side effect profile associated with interferon, ribavirin and first-generation DAAs caused debilitating symptoms and adversely affected patient-reported outcomes.
More recently, there have been significant gains in developing treatment regimens with high efficacy, low side effect profiles and less complex administration, particularly with the advent of interferon and ribavirin free regimens. There are numerous DAAs available on the market which can be prescribed depending on the genotype variant and state of disease progression, although these regimens are generally very expensive.
Boceprevir is a protease inhibitor that binds to NS3 and, like other protease inhibitors, must be given with PEG-IFN and RBV to minimize the emergence of viral resistance. The SPRINT-2 double-blinded study investigated whether the addition of boceprevir to standard therapy could improve the rates of sustained virologic response in previously untreated patients infected with HCV genotype 1. A total of 1246 and 226 patients were screened in the non-black cohort and the black cohort respectively, and were randomly assigned to one of three groups. In all three groups, PEG-IFN-α 2b and RBV were administered for 4 weeks (the lead-in period). Subsequently, group 1 (the control group) received placebo plus PEG-IFN and RBV for 44 weeks; group 2 received boceprevir plus PEG-IFN and RBV for 24 weeks, and those with a detectable HCV
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
level between weeks 8 and 24 received placebo plus PEG-IFN and RBV for an additional 20 weeks; and group 3 received boceprevir plus PEG-IFN and RBV for 44 weeks. The addition of boceprevir to standard therapy increased the SVR rates in previously untreated adults with chronic HCV genotype 1 infection. Among non-blacks, SVR rate was 40% with the standard of care and was significantly higher (P<0.001) in both boceprevir groups - 67% in group 2 and 68% in group 3. Among blacks, the SVR rate was 23% in group 1, 42% in group 2 (P=0.04, vs. group 1), and 53% in group 3 (P=0.004, vs. group 1).
Telaprevir is a NS3/4A serine protease inhibitor. In the ADVANCE trial, an international, phase 3, randomized, double-blind, placebo-controlled trial, 1088 patients with HCV genotype 1 infection who were treatment naïve were assigned to one of three groups: telaprevir combined with PEG-IFN-α 2b and RBV for 12 weeks (T12PR group), followed by PEG-IFN and RBV alone for 12 weeks if HCV
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
was undetectable at weeks 4 and 12 or for 36 weeks if HCV
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
was detectable at either time point; a group receiving telaprevir with PEG-IFN and RBV for 8 weeks and placebo with PEG-IFN and RBV for 4 weeks (T8PR group), followed by 12 or 36 weeks of PEG-IFN and RBV on the basis of the same HCV
RNA
Ribonucleic Acid (RNA)
The biological molecule that contains long chains of nucleotide units of a nitrogenous base, a ribose sugar and a phosphate is known as Ribonucleic acid. RNA is single stranded molecule with ribose, unlike DNA that is double stranded with deoxyribose. Another difference between a DNA and RNA molecule is presence of base uracil instead of thymine in RNA.
criteria; or a group receiving placebo with PEG-IFN and RBV for 12 weeks, followed by 36 weeks of PEG-IFN and RBV (PR group). Significantly more patients in the T12PR or T8PR group than in the PR group had a SVR (75% and 69%, respectively vs. 44%; P<0.001 for the comparison of the T12PR or T8PR group with the PR group). A total of 58% of the patients treated with telaprevir were eligible to receive 24 weeks of total treatment. Anaemia, gastrointestinal side effects, and skin rashes occurred at a higher incidence among patients receiving telaprevir than among those receiving PEG-IFN and RBV alone.
Sofosbuvir is a nucleotide analogue NS5B polymerase inhibitor with similar in vitro activity against all HCV genotypes. Two phase 3 studies, FISSION and NEUTRINO, investigated the addition of sofosbuvir to combination therapy in previously untreated patients with HCV infection. One was a single-group, open-label study, in which a 12-week regimen of sofosbuvir plus PEG-IFN-α 2b and RBV was investigated in 327 patients with HCV genotype 1, 4, 5, or 6 (of whom 98% had genotype 1 or 4). The other was non-inferiority trial, in which 499 patients with HCV genotype 2 or 3 infection were randomly assigned to receive sofosbuvir plus RBV for 12 weeks or PEG-IFN-α 2b and RBV for 24 weeks. In both studies, the primary end point was SVR at 12 weeks after the end of therapy. In the single-group study, a SVR was reported in 90% of patients with predominantly genotype 1 or 4 HCV infection. In the non-inferiority trial, a SVR was reported in 67% of patients in both the sofosbuvir plus RBV group and the PEG-IFN and RBV group. Response rates in the sofosbuvir–RBV group were lower among patients with genotype 3 infection than among those with genotype2 infection (56% vs. 97%). Adverse events (including fatigue, headache, nausea and neutropenia) were less common with sofosbuvir than with PEG-IFN.
Interferon-free regimens are being increasingly used to treat HCV infections with reduced toxicity. Simeprevir is an oral NS3/4A protease inhibitor with potent antiviral activity in patients infected with genotype 1 as well as antiviral activity demonstrated against isolates of genotypes 2, 4, 5, and 6. In the COSMOS trial, the efficacy of combined simeprevir and sofosbuvir was investigated. Patients with chronic HCV genotype 1 infections were enrolled who had previously not responded to PEG-IFN and RBV or were treatment naïve. Patients were randomly assigned in a 2:1:2:1 ratio to receive 150 mg simeprevir and 400 mg sofosbuvir daily for 24 weeks with (group 1) or without (group 2) RBV or for 12 weeks with (group 3) or without (group 4) RBV, in two cohorts: previous non-responders with METAVIR scores F0–F2 (cohort 1) and previous non-responders and treatment-naive patients with METAVIR scores F3–F4 (cohort 2). The primary endpoint was SVR 12 weeks after stopping treatment (SVR12). 168 patients were enrolled and randomised, and 167 started treatment (n=80 in cohort 1 and n=87 in cohort 2). SVR12 was achieved in 92% patients in cohort 1 and 94% in cohort 2. The most common adverse events in the pooled groups were fatigue (31%), headache (20%) and nausea (16%).
Ledipasvir is a NS5A nucleotide polymerase inhibitor with potent antiviral activity against HCV genotypes 1a and 1b. In the ION-1 trial, a phase 3, open-label study involving previously untreated patients with chronic HCV genotype 1 infection, patients were randomised in a 1:1:1:1 ratio to receive ledipasvir and sofosbuvir once daily for 12 weeks, ledipasvir–sofosbuvir plus RBV for 12 weeks, ledipasvir–sofosbuvir for 24 weeks, or ledipasvir–sofosbuvir plus RBV for 24 weeks. The SVR rates were 99% in the group that received 12 weeks of ledipasvir–sofosbuvir; 97% in the group that received 12 weeks of ledipasvir–sofosbuvir plus RBV; 98% in the group that received 24 weeks of ledipasvir–sofosbuvir; and 99 in the group that received 24 weeks of ledipasvir–sofosbuvir plus RBV. The most common adverse events were fatigue, headache, insomnia, and nausea. Once-daily ledipasvir–sofosbuvir with or without RBV for 12 or 24 weeks was highly effective in previously untreated patients with HCV genotype 1 infection.
Velpatasvir is a NS5A inhibitor with antiviral activity against HCV replicons in genotypes 1 – 6. In the ASTRAL-1 trial, a phase 3, double-blind, placebo-controlled study involving untreated and previously treated patients with chronic HCV genotypes 1, 2, 4, 5 or 6, including those with compensated
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
. Patients with HCV genotype 1, 2, 4 or 6 were randomly assigned in a 5:1 ratio to receive sofosbuvir and velpatasvir once-daily or matching placebo for 12 weeks. Because of the low prevalence of genotype 5 in the study regions, patients with genotype 5 did not undergo randomization but were assigned to the sofosbuvir–velpatasvir group. Of the 624 patients who received treatment with sofosbuvir–velpatasvir, 34% had HCV genotype 1a, 19% genotype 1b, 17% genotype 2, 19% genotype 4, 6% genotype 5, and 7% genotype 6. The SVR rate among patients receiving sofosbuvir–velpatasvir was 99%. Two patients receiving sofosbuvir–velpatasvir, both with HCV genotype 1, had a virologic relapse. None of the 116 patients receiving placebo had a SVR. Serious adverse events were reported in 2 of patients in the sofosbuvir–velpatasvir group and none in the placebo group. Once-daily sofosbuvir–velpatasvir for 12 weeks provided high rates of sustained virologic response among both previously treated and untreated patients infected with HCV genotype 1, 2, 4, 5, or 6, including those with compensated
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
.
Voxilaprevir is a NS3/4A protease inhibitor with potent antiviral activity against HCV genotypes 1-6. There were two phase 3 trials conducted involving patients who had been previously treated with a DAA-containing regimen. In POLARIS-1, patients with HCV genotype 1 infection who had previously received a regimen containing an NS5A inhibitor were randomly assigned in a 1:1 ratio to receive either sofosbuvir and velpatasvir plus voxilaprevir (150 patients) or matching placebo (150 patients) once daily for 12 weeks. Patients who were infected with HCV genotypes other than 1 (114 patients) were enrolled in the sofosbuvir–velpatasvir–voxilaprevir group. The SVR rate was 96% with sofosbuvir–velpatasvir–voxilaprevir, as compared with 0% with placebo. In the POLARIS-4 trial, patients with HCV genotype 1, 2, or 3 infection who had previously received a DAA regimen but not an NS5A inhibitor were randomly assigned in a 1:1 ratio to receive sofosbuvir–velpatasvir–voxilaprevir (163 patients) or sofosbuvir–velpatasvir (151 patients) for 12 weeks. An additional 19 patients with HCV genotype 4 infection were enrolled in the sofosbuvir–velpatasvir–voxilaprevir group. In this trial, the SVR rate was 98% with sofosbuvir–velpatasvir–voxilaprevir and 90% with sofosbuvir–velpatasvir. The most common adverse events were headache, fatigue, diarrhea, and nausea. In the active-treatment groups in both trials, the percentage of patients who discontinued treatment owing to adverse events was 1% or lower. Sofosbuvir–velpatasvir–voxilaprevir taken for 12 weeks provided high rates of sustained virologic response among patients across HCV genotypes in whom treatment with a DAA regimen had previously failed.
ABT-450 is an HCV NS3/4A protease inhibitor and is administered with low-dose ritonavir, an inhibitor of the cytochrome P-450 enzyme CYP3A4 as a pharmacologic enhancer (ABT-450/r). Ombitasvir is an HCV NS5A inhibitor and dasabuvir is a NS5B polymerase inhibitor. Together, this combination is known as the 3D Regimen. In the SAPPHIRE-I multicenter, randomized, double-blind, placebo-controlled trial, previously untreated patients with HCV genotype 1 infection were randomised in a 3:1 ratio to an active regimen consisting of ABT-450/r–ombitasvir and dasabuvir with RBV (group A) or matching placebos (group B). Patients received the study treatment during a 12-week double-blind period. The primary analysis compared the response rate in group A with the response rate (78%) in a historical control group of previously untreated patients without
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
who received telaprevir with PEG-IFN and RBV. A total of 631 patients received at least one dose of the study drugs. The SVR rate in group A was 96.2%, which was superior to the historical control rate. The response rates in group A were 95.3% among patients with HCV genotype 1a infection and 98.0% among those with HCV genotype 1b infection. The rate of discontinuation due to adverse events was 0.6% in each study group. Nausea, pruritus, insomnia, diarrhea, and asthenia occurred in significantly more patients in group A than in group B. In previously untreated patients with HCV genotype 1 infection and no
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
, a 12-week multi-targeted regimen of ABT-450/r–ombitasvir and dasabuvir with ribavirin was highly effective and was associated with a low rate of treatment discontinuation.
Transplant
In patients who have progressed to HCV-related
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
, a liver transplantation is the only available treatment option and this may also the case for patients with early stage hepatocellular carcinoma. HCV reinfection of the graft is almost inevitable however, and a majority of patients will show signs of
hepatitis and
cirrhosis
Cirrhosis
Dysfuntction of the liver due to various forms of damage which is usually characterized by scar tissue forming in the liver as well as fluid buildup in the abdomen.
.
Vaccine
Due to the high mutation rate and evolution of diverse viral variants (see Genetics), efforts to develop a vaccine against HCV have so far proved unsuccessful. A greater understanding of the cellular and humoral immunity against HCV will be critical in the development of a safe and effective vaccine. This includes understanding the potential for antibody cross-reactivity among genetically diverse isolates and how HCV inactivates primed CD4+ T helper cells even after they have contributed to the transient control of viraemia.
Epidemiology
HCV is a globally prevalent
pathogen
Pathogen
A biological agent such as viruses, bacteria or fungi that cause a disease.
and a leading cause of death and morbidity, with an increased seroprevalence over the past 15 years now estimated at 2.8%. This equates to > 185 million HCV infected people worldwide. New infections are estimated to occur at a rate of 1 - 3 cases per 100,000 persons per year; however the actual incidence is likely much higher as most new infections are asymptomatic. Genotypes 1a, 1b and 3 account for the majority of infections worldwide. In the United States, genotype 1 is the most common, accounting for approximately 70% of infection, followed by genotypes 2 and 3. Genotypes 4 and 5 occur primarily in Africa, genotype 6 mainly in Asia and only one genotype 7 infection has been reported; isolated in Canada from a Central African immigrant. Overall, genotypes 1a, 1b, 2a, and 3a are widely distributed across the globe and account for a large proportion of HCV infections in high-income countries.
There is a large degree of geographic variability in the worldwide distribution of HCV. Prevalence is highest in Africa and Asia, while prevalence is lower in the industrialised nations in North America, northern and Western Europe, and Australia. Nations in the developed world with relatively low rates of HCV seroprevalence include Germany (0.6%), Canada (0.8%), France (1.1%) and Australia (1.1%). Slightly higher seroprevalence rates have been reported in the USA (1.8%), Japan (1.5–2.3%) and Italy (2.2%). In China, there is a reported seroprevalence of 3.2%. In India, an overall rate of 0.9% was observed in one survey while in Pakistan there was a reported range between 2.4%-6.5%. The rate in Indonesia is 2.1% which is based on serosurveys of voluntary blood donors. Egypt has the highest rate of infection, with an estimated seropositive population of 73 million. Widespread transmission in Egypt is believed to have resulted contaminated glass syringes used in nationwide schistosomiasis treatment campaigns between 1960 and 1987.
Before serological screening of blood products was initiated, hepatitis C was most commonly transmitted by transfusion of contaminated blood products, but now it is acquired primarily via intravenous drug use. The rate of transmission following a needle-stick injury involving infected blood ranged from 0-10% in various studies, although this rate may be influenced by the size of the inoculum, the needle itself and the depth of inoculation. Needle sharing by people who inject drugs (PWIDs) is the primary mode of HCV transmission in the developed world. In countries such as the USA and Australia, where seroprevalence is highest among the middle-aged population, injectable drug use has been the dominant mode of transmission over the past few decades, accounting for 68% and 80% of current infections, respectively. Studies have also confirmed injectable drug use as the most common risk factor for HCV infection in prison inmates. In correctional institutions, which house a disproportionately higher number of PWIDs, HCV prevalence is substantially higher than it is in the general population, approximately 39% vs.1.8% in the general public. Sexual and perinatal (from mother to infant) transmission of HCV can also occur, however these are relatively infrequent compared to transmission of HBV and HIV.
Looking at demographics in the United States, 65% of subjects with anti-HCV antibodies were between 30 and 49 years of age. The prevalence of HCV antibody carriage was 2.5% in males compared to 1.2% in females. As factors such as age and sex appear to be important sources of variation in rates of disease progression, these may have important implications with regards to treatment decisions. Ethnicity and socioeconomic status also appear to be key factors. 3.2% of subjects with anti-HCV antibodies were reported in the African American population and 2.1% in Hispanics, compared to 1.5% in Non-Hispanic whites. In those below the poverty level, 3.2% were seroprevalent compared to 1.6% in those above the poverty level.
Additional Resources

The Hepatitis C Trust
The Hepatitis C Trust is the national UK charity for hepatitis C with offices in London and Falkirk. It has been operating since 2001. It is a patient-led and patient-run organisation: most of their board, staff, and volunteers have had hepatitis C and have cleared it after treatment.
http://www.hepctrust.org.uk/

British Liver Trust
The British Liver Trust is the leading UK charity for adults with all types of liver disease.They are determined to achieve real change in liver health. Most conditions such as stroke, lung disease, heart disease and most types of cancer have seen death rates decline dramatically over the last 40 years yet we are facing a liver disease crisis in the UK with the numbers affected increasing at an alarming rate. Their key areas of their work are:
• Supporting those affected by liver disease
• Raising awareness of how liver disease can be prevented and promoting early detection of those with a problem
• Campaigning for better and more equitable services
• Supporting patient focused research
https://www.britishlivertrust.org.uk/
LIVERrNORTH
LIVErNORTH is a national liver patient support group based at the Freeman Hospital in Newcastle upon Tyne. Whatever liver disease you may have, they are here to support you. They are run entirely by unpaid volunteers and all of their services are absolutely free to UK liver patients, their carers and families.
http://www.livernorth.org.uk/
References
- "Cerny, A., & Chisari, F. V. (1999). Pathogenesis of chronic hepatitis C: immunological features of hepatic injury and viral persistence. Hepatology, 30(3), 595-601."
- "Thimme, R., et al. (2001). Determinants of viral clearance and persistence during acute hepatitis C virus infection. The Journal of experimental medicine, 194(10), 1395-1406"
- "Thomas, D. L., et al. (2000). The natural history of hepatitis C virus infection: host, viral, and environmental factors. Jama, 284(4), 450-456."
- "Lauer, G. M., & Walker, B. D. (2001). Hepatitis C virus infection. New England journal of medicine, 345(1), 41-52."
- "Salomon, J. A., et al. (2003). Cost-effectiveness of treatment for chronic hepatitis C infection in an evolving patient population. Jama, 290(2), 228-237."
- "Afdhal, N. H. (2004) The natural history of hepatitis C. Seminars in liver disease, 24(2), 3-8."
- "Bowen, D. G., & Walker, C. M. (2005). Adaptive immune responses in acute and chronic hepatitis C virus infection. Nature, 436(7053), 946-952."
- "Shepard, C. W., et al. (2005). Global epidemiology of hepatitis C virus infection. The Lancet infectious diseases, 5(9), 558-567"
- "Bowen, D. G., & Walker, C. M. (2005). The origin of quasispecies: cause or consequence of chronic hepatitis C viral infection?. Journal of hepatology, 42(3), 408-417"
- "Messina, J. P., et al. (2015). Global distribution and prevalence of hepatitis C virus genotypes. Hepatology, 61(1), 77-87."
- "Younossi, Z., & Henry, L. (2015). Systematic review: patient‐reported outcomes in chronic hepatitis C‐the impact of liver disease and new treatment regimens. Alimentary pharmacology & therapeutics, 41(6), 497-520."
- "Dubuisson, J. (2007). Hepatitis C virus proteins. World journal of gastroenterology, 13(17), 2406."
- "Poordad, F., et al. (2011). Boceprevir for untreated chronic HCV genotype 1 infection. New England Journal of Medicine, 364(13), 1195-1206."
- "Jacobson, I. M., et al. (2011). Telaprevir for previously untreated chronic hepatitis C virus infection. New England Journal of Medicine, 364(25), 2405-2416"
- "Lawitz, E., et al. (2013). Sofosbuvir for previously untreated chronic hepatitis C infection. New England Journal of Medicine, 368(20), 1878-1887."
- "Lawitz, E., et al. (2014). Simeprevir plus sofosbuvir, with or without ribavirin, to treat chronic infection with hepatitis C virus genotype 1 in non-responders to pegylated interferon and ribavirin and treatment-naive patients: the COSMOS randomised study. The Lancet, 384(9956), 1756-1765."
- "Afdhal, N., et al. (2014). Ledipasvir and sofosbuvir for untreated HCV genotype 1 infection. New England Journal of Medicine, 370(20), 1889-1898."
- "Feld, J. J., et al. (2015). Sofosbuvir and velpatasvir for HCV genotype 1, 2, 4, 5, and 6 infection. New England Journal of Medicine, 373(27), 2599-2607."
- "Bourlière, M., et al. (2017). Sofosbuvir, velpatasvir, and voxilaprevir for previously treated HCV infection. New England Journal of Medicine, 376(22), 2134-2146."
- "Zeuzem, S., et al. (2014). Retreatment of HCV with ABT-450/r–ombitasvir and dasabuvir with ribavirin. New England Journal of Medicine, 370(17), 1604-1614."